PTPN’s comprehensive Quality Assurance Program helps ensure appropriate treatment and monitors for overutilization.
Our credentialing program ensures — at no cost to you — that every PTPN provider meets the highest quality standards in the industry. Our member providers must meet strict credentialing requirements that exceed other networks’ and state licensing requirements, and surpass those that such accrediting bodies as the NCQA (National Commission for Quality Assurance) require for physicians in managed care plans. And PTPN is the only outpatient rehab network that performs on-site inspections as part of the credentialing and re-credentialing process.
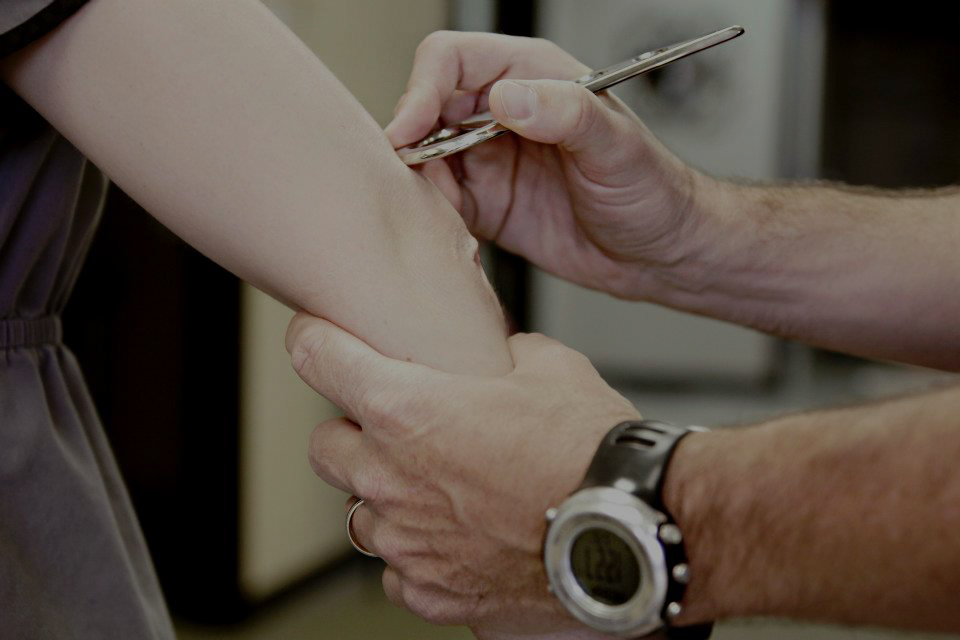
Our unparalleled utilization review program serves as your watchdog, reviewing cases to make sure that treatment matches the needs of the patient and that treatment is producing the desired clinical outcome. PTPN’s utilization management team continually monitors, evaluates and optimizes health care resource utilization within the network.